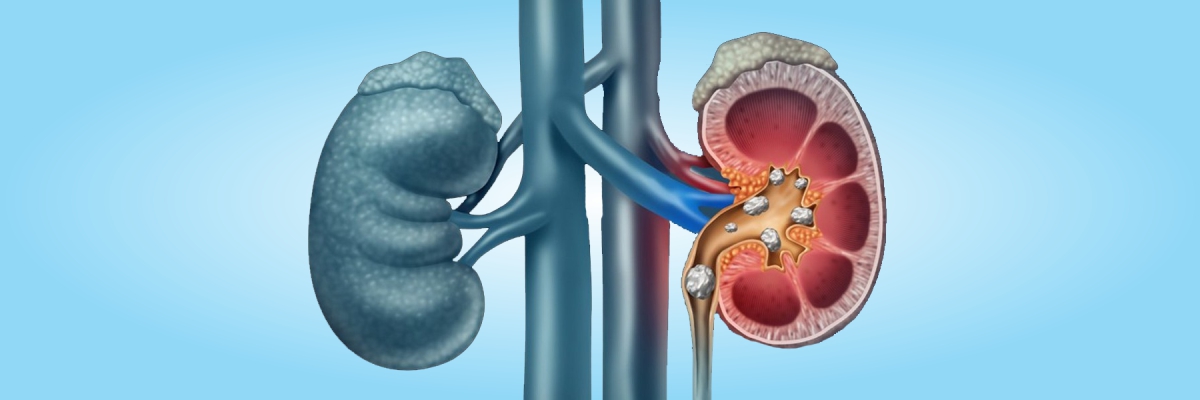
Kidney Stones
The stones may be small and pass unnoticed through the urinary tract, but they can also cause extreme pain as they leave the body.Symptoms
A kidney stone usually remains symptomless until it moves into the ureter. When symptoms of kidney stones become apparent, they commonly include:
- severe pain in the groin and/or side.
- blood in urine.
- vomiting and nausea.
- white blood cells or pus in the urine.
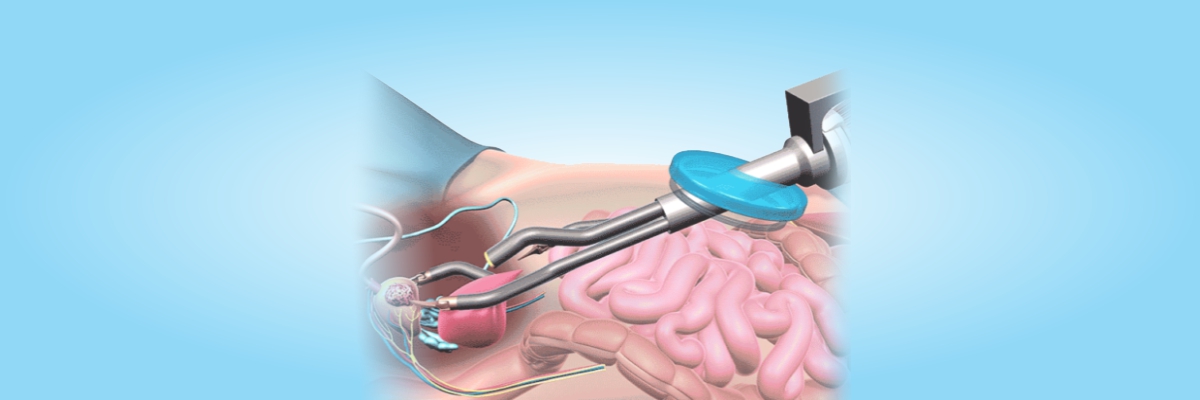
PCNL
Percutaneous nephrolithotomy is the most commonly employed minimally invasive kidney stone removal surgery. Typically it is used for stones more than 2 cm and can be done under spinal or general anesthesia. A small incision less than 1 cm is made. A nephroscope is then passed into the kidney and the stone is fragmented into small pieces and removed. A DJ stent is then placed in the kidney.
RIRS (RETROGRADE INTRA-RENAL SURGERY)
In this technique, a flexible ureteroscope is passed through the urinary passage, through the bladder into the kidney directly. Using a Holmium laser, under direct vision the kidney stones can be broken into small fragments and removed with miniature baskets. No cut in the skin is given in this procedure. It is especially useful to remove stones in difficult locations inside the kidney. There are minimal bleeding and early recovery of patients using this technique. If you are looking for the best kidney stone treatment in Bathinda visit Dr. Sameer Grover, with 15 years of experience in the field of urology and surgical procedure. He follows a considerate approach and has delivered more than 5,000 successful surgeries.
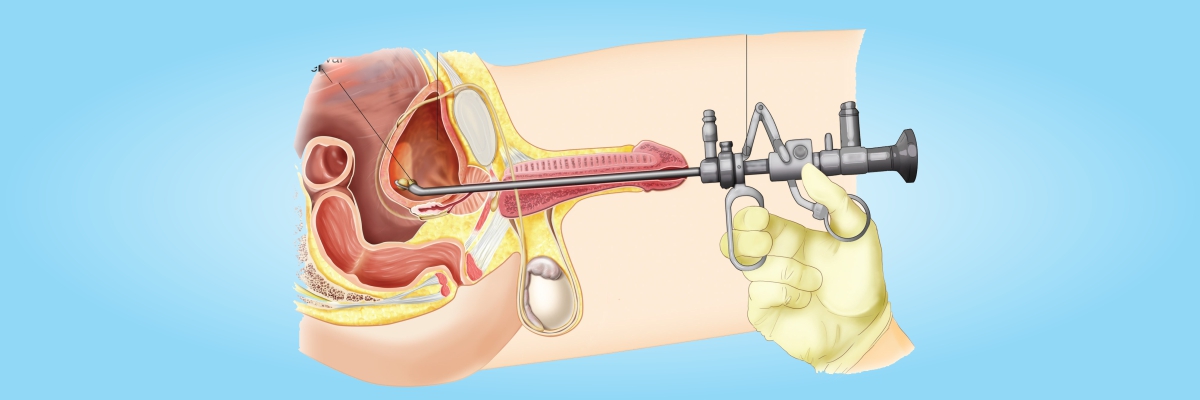
URS(URETERO-RENOSCOPY)
Stones that are stuck in ureters( a thin tube that carries urine from kidney to the bladder) are treated using a rigid ureteroscope which is as thin as a pen. The ureteroscope is passed through the urinary passage and no cut is given on the skin. Once the ureteroscope reaches up to the stone, it is fragmented into small pieces using Holmium laser or a pneumatic lithoclast. The stone fragments are ten removed using a forceps. At the end of the procedure, a stent is placed in the ureter which is but a safety device. The stent is removed around a week later through the urinary passage.
BLADDER STONE TREATMENT
Bladder stones commonly form in the bladder due to some obstruction to outflow of urine. More common in males this can be due to narrowing of urethral passage ( stricture urethra) or commonly due to an enlarged prostate.In such cases the obstruction due to prostate enlargement also needs to be treated surgically. Uncommonly stones that pass down from the kidneys into the bladder can also grow in size over years.
TREATMENTS CYSTOLITHOLAPAXY
In this procedure , a cystoscope is passed through natural urinary passage into the bladder to visualize the stone.After this the stone is broken into small pieces with either laser or hand held pneumatic lithoclast. Stone fragments are then removed. After the procedure a urinary catheter is left inside for a day or two. This surgery can be done as a day care procedure.
TURP (TRANS URETHRAL RESECTION OF PROSTATE)
Patients who have difficulty in passing urine or have retention of urine due to an enlarged prostate are treated by transurethral resection of the prostate. This surgery can be done under spinal or general anesthesia. There is no cut involved on the skin. Using a cystoscope, the prostate is directly visualized and then using a resectoscope and electric current, prostate tissue is scooped out. At the end of the surgery, a urinary catheter is placed for 2 to 4 days. Post removal of catheter patients will find that their urine flow has improved remarkably and the feeling of some urine remaining in the bladder after voiding has gone. Usually, the patient stays in the hospital for 1 to 2 days. This surgery is the gold standard for the treatment of benign prostatic hyperplasia.
Holmium Laser Prostrate surgery:
This is the latest technological refinement in prostate surgery. Patients with BPH are treated using a green laser through a cystoscope. The prostate tissue is evaporated using the green laser. This technique is especially useful for patients with heart disease who are on blood thinners such as aspirin or have a pacemaker. Prostate surgery can be done in these patients without stopping blood thinners or changing pacemaker settings. There is no to minimal bleeding in this surgery. In fact, it can even be done on a day-care basis, meaning that the patient need not be admitted to the hospital for overnight.
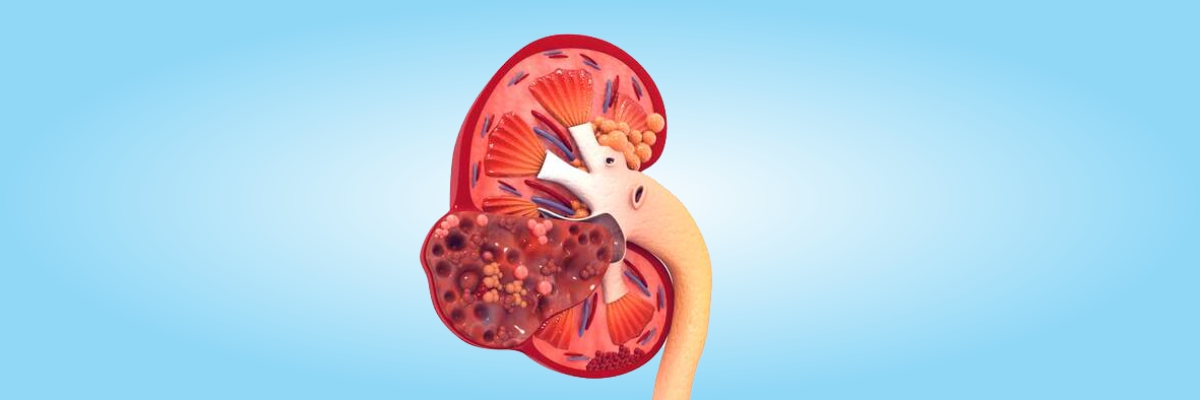
Kidney Cancer
Dr Sameer Grover has wide experience of handling cancers of urinary system.Cancer of the kidney was a dreadful disease in the past because usually patients use to present in late stages with advanced disease. In the present time most of kidney cancer are incidentally detected during ultrasound or other imaging studies done for unrelated problems. The other presenting symptoms of kidney cancer are pain in the flanks, blood in urine, a palpable mass. A contrast CT scan is required for confirming doubts about the presence of tumor. Surgery is the only realistic treatment of this disease. With the advancement of technology, these tumors can be dealt with minimally-invasive surgeries or in-common parlance key hole surgeries. The hospital stay can be as short as one day only and people can resume their normal work in three to five days time.
- RADICAL NEPHRECTOMY
Using laparoscopic approach the entire kidney along with the tumor is removed and sent for the biopsy. 1. Open 2. Laparoscopic
- PARTIAL NEPHRECTOMY
If the tumor is very small then sometimes it is possible to remove only the tumor and the kidney can be saved. The results of this surgery are comparable to removing the entire kidney. In this surgery also hospital stay is short and recovery is fast.
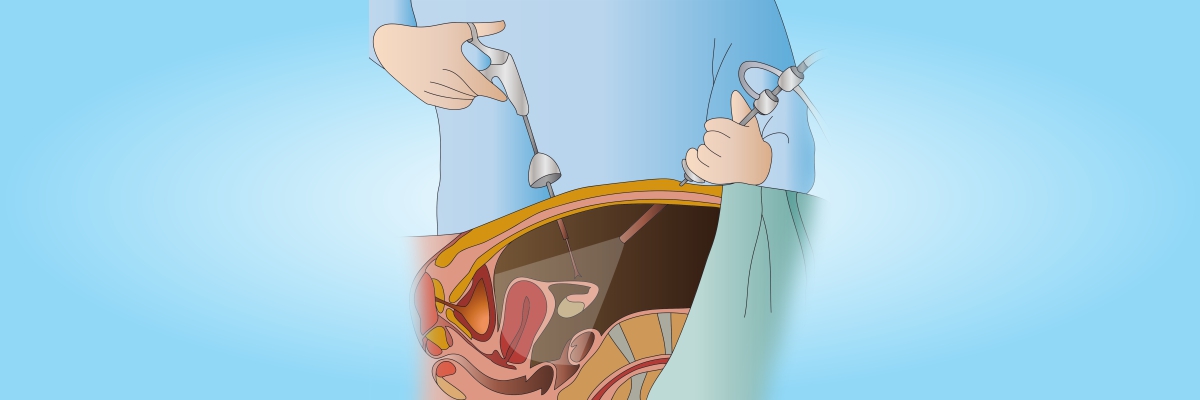
Laparoscopic Urologic Surgery
Laparoscopic urologic surgery is a surgery where a doctor corrects urological issues without causing much agony to the patient. It is a minimally invasive surgery that involves the use of a laparoscope which has an inbuilt camera and several long and thin surgical instruments. It is inserted into the body through small incisions. With this surgery, patients experience a much better post-operative pain control, short hospitalization, quick recovery period and better results. Nowadays, robotic technology is implemented in laparoscopic urologic surgery. Robotic surgery provides much better visualization and enhanced dexterity to the surgeon. Robotic technology has gained popularity especially in radical prostatectomy for prostate cancer.
What Are the Advantages of Laparoscopic Urological Surgery?
- Reduced Bleeding
This reduces the chances of requiring a blood transfusion.
- Smaller Incision:
This not only reduces pain but also shortens recovery time, resulting in less post-surgery scarring and surgery marks.
- Less Pain
Because it is a minimally invasive surgery, patients experience minimal pain.
- Less Hospital Stay
Although the surgery time is usually slightly longer, the hospital stay is comparatively less in this surgery. In many cases, the patient is discharged the same day.
- Reduced Risk of Catching Infections:
The surgery decreases the exposure of internal organs to external contaminants thereby reducing the risk of catching infections.
Andrology
Andrology & Urology centre is an exclusive centre for Male Infertility, Sexual Dysfunction & Men’s Health. It is a one stop solution for all men’s reproductive problems under one roof. Found with a vision of providing outstanding patient care based upon the principles of cooperation, compassion and innovation, this centre is well known for its strict adherence to international standards and quality. Here we offer latest techniques in this rapidly changing sub specialty, which makes us one of the Punjab’s premier male reproductive centre.
What Andrology Entails
Andrology deals with the following issues of men's health.
- Infertility
Of all the infertility issues, around 50% cases are due to male-factor infertility. Seeking help from an Andrologist who is specialized in providing proper and timely treatment for all male-factor infertility related issues would be a better option.
- Erectile Dysfunction
The inability to achieve or maintain an erection while having intercourse is known as erectile dysfunction. Men may find it difficult to deal with this situation. However, with appropriate treatment taken at the right time, this condition can be treated.
- Prostate Disease
Prostate problems are common in men over the age of 50. The prostate is a gland that is associated with semen production in men. Prostate gland enlargement, prostatitis, and prostate cancer are some of the common disease associated with this gland.
- Male Hormone Deficiency
Any deficiency in male hormones or androgens, which plays an essential role in giving men the male attributes, can lead to a lot many other health-related issues. Consulting an andrologist can help one find the exact cause and effective solution.

Male Infertility
Male factor contributes around 50% to the infertility cases though unfortunately in Indian scenario it is uncommon for males to accept it. A proper evaluation of male partner is necessary in all couples facing infertility. It begins with the simple physical examination followed by the semen analysis and hormonal analysis. Depending upon the examination and reports a diagnosis can be made of obstructive or non-obstructive azoospermia.
Treatment
- Obstructive Azoospermia
- VEA (VASO-EPIDIDYMAL ANASTOMOSIS)
- PESA
- TESA
- Micro-TESSE
Erectile Dysfunction
A type of sexual dysfunction in which an erection of the penis cannot be maintained or achieved during sexual activity is known as erectile dysfunction (ED).
Causes of Erectile Dysfunction
Erectile dysfunction occurs due to obesity and metabolic syndrome. Blood pressure, body composition, and cholesterol can be altered by obesity and metabolic dysfunction that may lead to erectile dysfunction. Erectile dysfunction can also occur due to Parkinson’s disease, alcoholism, Peyronie’s disease, multiple sclerosis disease, sleep disorders, and drug abuse.
Symptoms
A man’s inability during sexual intercourse to get a firm erection is the main symptom of erectile dysfunction. The early symptoms of erectile dysfunction are trouble keeping an erection, trouble getting an erection, and decreased sexual desire.
Preventing Erectile Dysfunction
Certain factors increase the chances of erectile dysfunction. Avoiding these factors and maintaining good overall health can help in preventing erectile dysfunction. Following are some of the common recommendations:
- Quit smoking.
- Avoid drinking alcohol.
- Eat a balanced diet.
- Maintain ideal weight.
- Go for regular health check-ups.
- Stress and anxiety must not be ignored, get professional help.
- Exercise daily or involve yourself in physical activities frequently.
- Some medication such as tranquilizers and immunomodulators can also lead to erectile dysfunction.
Diagnosis
The common treatments for erectile dysfunction include:
- Medication:
Oral medications or injectables can be suggested, which help in stimulating the body’s natural erectile mechanism. These may not be equally effective for all.
- Hormone Replacement Therapy:
Hypogonadism is a condition that develops over time and can be defined as a diminished production of sex hormones. Certain medications and medical conditions can lead to this condition. Topical gels and injections can be used to improve the count of male sex hormones.
- Lifestyle Modifications:
As mentioned earlier, lifestyle habits such as smoking and drinking alcohol are some of the most common reasons for erectile dysfunction. Similarly, chronic stress or depression can also cause this problem. Living an active and healthy lifestyle can help in reversing this condition in many cases.
- Surgical Treatment:
A penile prosthesis is an effective solution for erectile dysfunction if medical therapy fails to show results. The majority of patients get satisfactory results with this treatment.

Reconstructive Urology
Reconstructive urology is a specialized field in urology which focuses on restoring both the structure and functions of the genitourinary tract. Some of the conditions which can necessitate reconstructive surgery are prostate procedures, full or partial hysterectomies, trauma such as industrial accidents, straddle injuries, etc. urethral strictures and sometimes childbirth. Surgeons should have extensive expertise in performing complex reconstructive surgery on the kidney, ureter, bladder, urethra and male genitals. Some of the common reconstructive surgery procedures include:
- Urethral disruption injuries caused by fractured pelvis.
- Recto-urinary fistulas following prostatectomy or pelvic surgery.
- Refractory male urethral strictures and radiation-induced urinary fistulas.
- Major bladder reconstruction.
- Major ureter reconstruction.
- Vesicovaginal or ureterovaginal fistulas after pelvic surgery.
- Male urinary incontinence.
- Peyronie’s disease.
Endo Urology
This is a method whereby most of the urinary surgeries are performed by passing telescopes through normal urinary openings without giving any cuts in the body. This method can take care of most of the urinary problems like stones, bladder cancer, prostate enlargement (BPH), bleeding through urinary tract, etc. The common urological procedures are URS, PCNL, TURBT, TURP.
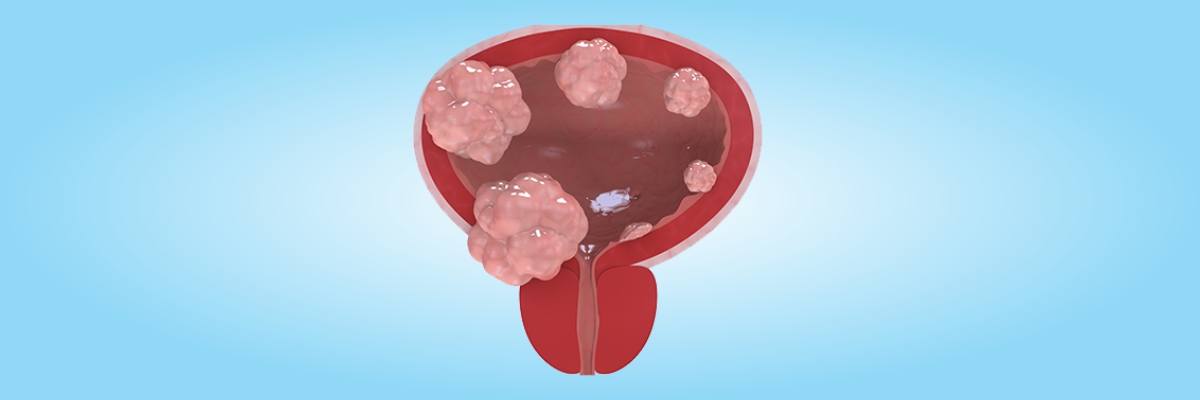
Bladder Cancer Treatment
Presence of blood in urine is the most common way in which bladder cancer presents. Some patients may also present with pain or burning during urination without any evidence of infection. Ultrasound or a CT scan along with urine cytology will confirm the presence of cancer. Unusually , small cancers can only be diagnosed by doing cystoscpoic evaluation of bladder.
TURBT(TRANS URETHRAL RESECTION OF BLADDER TUMOR)
The initial treatment of bladder cancer is trans-urethral resection of bladder tumor. Under general or spinal anesthesia, a thin tube called cystoscope is passed through urine passage into the bladder. The tumor is directly visualized and cut out and sent for biopsy. For small tumors which are not muscle invasive this is all that needs to be done. Patient however has to remain on strict follow up which involves ultrasound, urine cytology and cystoscopy every three months.
RADICAL CYSTECTOMY
For muscle invasive bladder tumors or extensive bladder tumors, the whole bladder is removed and a urinary diversion is created in the form of an ileal conduit or a neo-bladder using patient’s own intestines. This is a major surgery requiring 7 to 10 days of hospitalization.
RADIATION AND CHEMOTHERAPY
In advanced and metastatic diseases radiotherapy and chemotherapy are used in conjunction with surgery to achieve maximum control of disease.
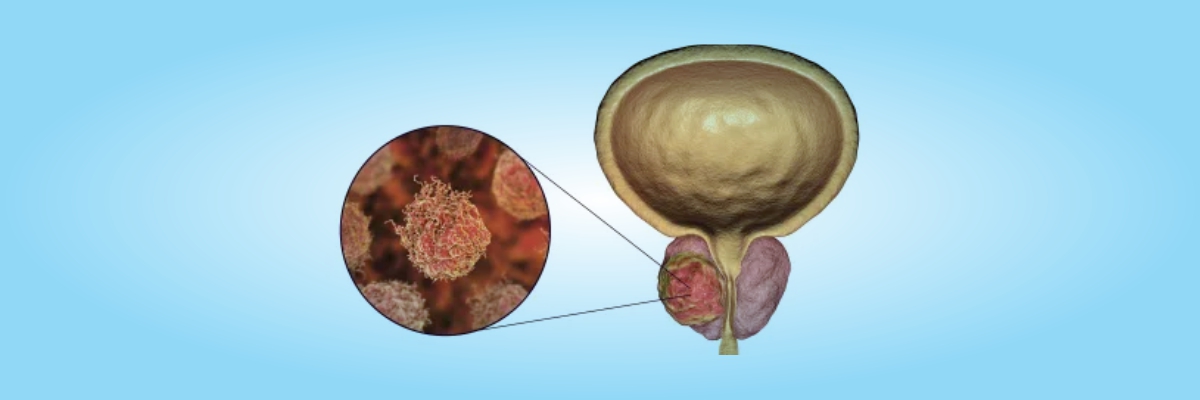
Prostate Cancer
Dr. Sameer Grover is a highly skilled well-trained urologic oncologists and one of the best Prostate Cancer Doctor in Bathinda.It is the most common cancer amongst men affecting about 1 million males in India every year. If detected early it can be treated.
What are the symptoms of prostate cancer?
n most cases, prostate cancer does not cause any symptoms. In fact, these days more and more cases of early prostate cancers are being detected because of the routinely prescribed PSA test by physicians as part of the annual health check up after a certain age.
Symptoms
- Decreased force of urination or a weak urinary stream.
- Straining to pass urine.
- Sense of incomplete emptying.
- Frequency of micturition.
- Urgent desire to pass urine, which may also be associated with incontinence at times.
- How can you treat prostate cancer?
- Depending on the stage of the cancer, age of the patient and the overall fitness levels of the patient, there are various prostate cancer treatment options available.
- Biopsy is done first and depending on the result surgical and other ( Harmonal therapy) options are offered to patients.
